Background to our survey: “A Survey of Current UK-wide use of the BASMI outcome measure in Axial Spondyloarthritis.”
Since the days of when people living with what is now known to be Axial Spondyloarthropathy (Axial SpA) being put into plaster casts (1950’s) to now; there has been a vast evolution in the knowledge and care both medically and within the world of physiotherapy for this condition. Having used the Bath AS Metrology Index (BASMI) with my patients over a number of years from the pre biologic days until now, I wonder if the BASMI is still serving a purpose for both clinicians and of course people living with Axial SpA?This blog looks at some of my own thoughts which led to the survey we devised on the current use of the BASMI in the UK which will hopefully act as a springboard for discussion and future research.
 The BASMI was devised by a group of physiotherapists, rheumatologists and people with lived experience to specifically look at the areas where reduction of movement occurs with AxSpA (Jenkinson et al 1994). Those who are familiar with it will know it measures 5 key movements: tragus to wall, lateral spinal side flexion, lumbar flexion, cervical rotation and hip abduction. It has excellent inter and intra-rater observer reliability (Martindale et al 2012) It is also used widely in clinical research trials as an outcome measure.
Elements of the BASMI are described by the Spondylitis International Society (ASAS) Sieper et al 2009.) And in 2016 an update of the ASAS-EULAR management recommendations for axial spondyloarthritis stated that monitoring should include a broad variety of assessments and cited the ASAS core set being still “guiding” whilst not using the acronym BASMI it did use the words “spinal mobility”. The latest NICE guidelines, 2017 for spondyloarthritis in over 16’s; diagnosis and management do not include any objective outcome measures looking at the range of movement.
One criticism stated over the years according to Braun et al 2014 is that it is not a pure spinal measure given that hip abduction is measured and not chest expansion. They suggest there is room for development of the BASMI to include other features. Other suggestions have been made such as measuring occiput to wall and also adapting the scoring system such as the 2-point score, Van Der Heijde et al 2008.
The BASMI was designed to be used in conjunction with the other BATH indices which are subjective questionnaires notably the BASDAI and BASFI. The BASMI now tends to be used in isolation which was not ithe original purpose and in some centres, it is not used at all. Gregory et al in 2017 looking at services in the North West for people living with spondyloarthritis found: “across our regional forum of physiotherapists there is a wide variation in how physiotherapy-led spondyloarthritis assessment is provided”. Also, in collaboration with the NASS a survey of rheumatology departments in 2018 found only 65% of the 83 respondents said their departments carried out the BASMI. Derakhshan et al 2018.

Another point I would like to make is that over the years thankfully with improved medication the deformities that we used to see are less frequent. A study by Rodriguez et al 2019 has shown “our findings indicate that long-term anti-TNF therapy decelerates the progression of structural damage in the SI joints”. They looked at the radiographic progression of early AxSpA with the use of anti-TNF for up to 6 years in patients. The BASMI is amongst other things measuring the progression of the disease but if this is being slowed by anti-TNF then does it still have a purpose?
Currently in my own practice as part of an assessment of a person with a new diagnosis of AxSpA the BASMI is completed to give a baseline measure of movement. This occurs in combination with subjective questioning and other objective findings such as functional movements. Clinical reasoning informs a management plan often advising on specific stretches and exercises for which the BASMI is a useful guide as to where movement is restricted. It is also useful depending on the person to look at the scoring table and explain where they sit with regard to their individual movements. A study in 2013 by Chilton-Mitchell et al looked at the BASMI on healthy individuals. They suggest that “The generation of normative values has the potential to inform clinical assessment of spinal mobility and assist patients in understanding how their spinal mobility compares with that of a healthy age-matched population” They found that it is unusual for this group (normal population) to score zero. It can be helpful for some people and reassuring that their movements are ok. Also, it can act as an incentive to advise people to stretch if they are stiffening and moving further up the table with worsening scores. If the stiffness we measure fits with their subjective experience this can also be powerful and by demonstrating this with the BASMI this can be an incentive to work on their specific stretches. For a new patient though I sometimes wonder is this scary for them to be measured and does it feed into negative thoughts about their bodies and concerns about deterioration of movement; hence my next train of thought…
Another reason for me to question the use of the BASMI in 2022 is in response to the narratives and discussions about non-specific low back pain. A clinical commentary paper by Bunzli et al 2017 is an interesting read talking about fear-related low back pain. I acknowledge this clinical presentation is very different to someone who has a diagnosis of Axial SpA which is a progressive autoimmune disease. However, I see two aspects here potentially at play. Firstly, does doing the BASMI and explaining the table to a newly diagnosed person feed into thoughts and concerns about losing range of movement in time and this escalates their worries and negative beliefs about their bodies feeding into pain mechanisms. Secondly, for established disease are we feeding into concerns at times looking at subtle changes when they could be age-related or from mechanical causes? This is potentially a controversial avenue of discussion as NSLBP and AxSpA are completely different presentations, but it is an important consideration I think to consider with our group.
This survey also seems timely to me given the recent “Rheumatology workforce: a crisis in numbers” British Society of rheumatology 2021. And the GIRFT report in rheumatology with their recommendations. Also, NHSE and NHS improvement in consultation with the BSR Clinical Affairs Committee published guidance on PIFU (patient-initiated follow-up) for adult rheumatology services. Plus, the NHS directive for more virtual consultations means overall, there is a real and necessary drive to make every appointment count. The AStretch team undertook a feasibility study in December 2020 looking at using a novel remote video-guided BASMI tool. They concluded that whilst it is unlikely to be a reliable and valid replacement they showed the feasibility and tolerability of this remote monitoring. This is encouraging given the research and development of app-based solutions for BASMI.
So, having discussed this with the AStretch committee we agreed that a UK-wide survey of the current use of the BASMI would act as a good springboard for us to start a conversation about current practice. This would in turn help us shape other questions we have in this area to guide future research questions and ultimately to advise on best practice. We hope then for example to devise and carry out surveys to ask questions of people living with AxSpA about their experiences of the BASMI. Firstly, we felt we need to establish what we are doing as clinicians in the UK.
The title: “A Survey of Current UK-wide use of the BASMI outcome measure in Axial Spondyloarthritis.” The survey was shared across multiple platforms and email professional distribution lists and was open from 2nd-12th October 2021. The aim was to find out when the BASMI was used, by whom, the reasons for it’s use and how the scores were recorded. Having agreed on potential reasons for doing the BASMI we decided on a scale and then the survey platform was able to rank these statements which meant we could extrapolate the most important reasons (table 1). We felt some free text options were also important to capture reasons we hadn’t considered. We added in chest expansion and free text to add any other regular measured areas. We also asked about confidence in carrying out the BASMI and how frequently it is done. Results: 74 UK healthcare professionals completed the survey; mostly it is physiotherapists who undertake the BASMI (69%), other clinicians also measure: nurses (10%), medics (9%), physiotherapy support workers (10%), healthcare support workers (2%). Confidence in performing the BASMI averaged at 3.5/5. Most respondents record the BASMI in the electronic record (73%), app-based solutions are developing (7%) and paper-only recording diminishing (20%). In terms of frequency most (73%) recorded “it depends” implying this is done on an individual patient basis. Table 1 presents data with regards to why the BASMI is undertaken, scored by participant ranking, and free text responses about reasons for use. Table 1: Participant ranking score summation for “reason to use the BASMI” and free text “reasons for use of the BASMI” | Item | Overall Rank | Total Score * | For all newly diagnosed patients | 1 | 555 | To help us devise a bespoke exercise plan | 2 | 513 | To address poor movement or function | 3 | 498 | To address/encourage adherence with exercise/advice | 4 | 451 | It’s part of their on-going management | 5 | 391 | Delay to diagnosis affecting start of treatment and therefore movement restrictions apparent | 6 | 356 | Guidelines suggest yearly monitoring | 7 | 332 | As an outcome measure pre and post hydrotherapy | 8 | 295 | To address an increase in pain levels | 9 | 277 | For patient preference | 10 | 265 | Rheumatology team asked for it | 11 | 202 | For research purposes / as a part of a clinical trial | 12 | 155 | * Score is a weighted calculation. Items ranked first are valued higher than the following ranks, the score is a sum of all weighted rank counts. | FREE TEXT REASONS FOR THE USE OF THE BASMI | Helpful to patients to objectively understand their movement. Newly diagnosed-baseline score at initial assessment. Pre/post hydrotherapy., To encourage a home exercise programme. Most objective of PROMs for AxSpA. Provides an indication on posture and flexibility. Objective measure that we can compare over time. To monitor any subclinical restrictions creeping in over time. Started biologics- see if improving / new baseline. Pre commencing biologic. Provides the basis on which to base a specific exercise programme. Patient request. To support new patients in identifying issues. To assess the progression of the disease over time. Key objective measure of spinal movement. |
Conclusions:
A large sample size for this survey implies a good level of interest to better understand the current application of the BASMI. It shows clinicians use the BASMI on newly diagnosed patients as a priority in their assessment and shared-decision making. Other aspects such as addressing poor movement and adherence to exercise are also ranked highly. The reported reasons for BASMI use are varied, and its application is not standardised across UK rheumatology teams. This might reflect the diverse trajectory of Axial SpA and the importance of seeing patients as individuals. How and why, we have undertaken physical outcome measures is crucial for consideration as we currently consider remote versus face-to-face consult pathways for our axSpA cohort as well as patient-initiated follow up’s. However, there is enough evidence here to recommend ongoing, regular application of the BASMI in a traditional face-to-face setting. Next steps will be to consider the patient perspective on this topic. As a first venture out into the world of designing a survey for me this has been an invaluable experience with the support of the AStretch team. Being able to draw upon a wide variety of clinical backgrounds and experience helped to shape this project and we have a robust survey as a result. The use of Twitter and other networking platforms to disseminate the survey was invaluable and I’m proud to say the poster and abstracts were accepted and shown at both the BSR and BritSpA 2022 conferences. 
Kate
NICE guideline [NG65]Published: 28 February 2017 Last updated: 02 June 2017: Spondyloarthritis in over 16s: diagnosis and management. Overview | Spondyloarthritis in over 16s: diagnosis and management | Guidance | NICE Samantha Bunzli, Anne Smith, Robert Schutze. Making Sense of Low Back Pain and Pain-Related Fear. Journal of Orthopaedic & Sports physical therapy. September 2017, volume 47 no 9 Braun J, Kiltz U, baraliakos X, Van der Heijde D. Optimization of rheumatology assessments the actual situation in axial spondylarthritis including ankylosing spondylitis. Clinical and experimental rheumatology. 2014 Vol 32, No 5. Supp 85 Lucy Chilton-Mitchell, Jane Martindale, Anna Hart and Lynne Goodacre. Normative values for the Bath Ankylosing Spondylitis Metrology Index in a UK population. Rheumatology. 2013; 52. 2086-2090 Derakhshan MH, Pathak H, Cook D, Dickinson S, Siebert S, Gaffney K. Services for spondyloarthritis: a survey of patients and rheumatologists. Rheumatology (Oxford) 2018;57:987–96 Gregory, W, McCall G, Shaw K, Martindale J,. Audit and clinical evaluation of the North West Spondyloarthritis physiotherapy services. Rheumatology 2017: 6: Supplement 2; E03 Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, Burgos-Vargas R, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009;68 Suppl 2:ii1–44. Van der Heijde D, Ramiro S, Landewé R, Baraliakos X, van den Bosch F, Sepriano A, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 2017;76:978–9 Van Der Heijde et al 2008. Proposal of a linear definition of the Bath Ankylosing Spondylitis Metrology Index and comparison with the 2 step and 10 step definitions. Annals of rheumatology disease. 67: 489-493
Home-BASMI: feasibility and tolerability of a remote-consult, video-delivered application of the BASMI (an early report)
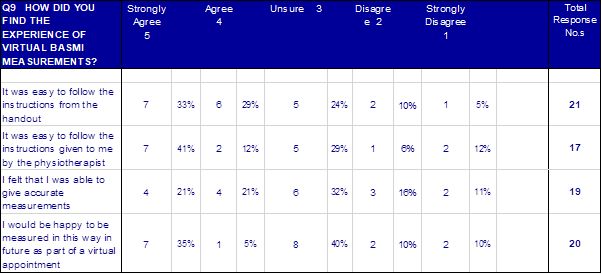
 December 2020 Introduction: Objective measurement of movements for people living with axial spondyloarthritis is a core part of care, especially so for physiotherapists. Whilst these measurements have no doubt been going on for longer than this, their standardisation was first popularised by the Bath Ankylosing Spondylitis Metrology Index (Jenkinson et al. 1994). The creation of the Bath indices stems from the work of a research team consisting of rheumatologists, physiotherapists, and research associates with a specialist interest in AS at the Royal National Hospital for Rheumatic Diseases (RNHRD). With respect to the functional and disease activity indices, the team obtained input from patients with AS. As a part of their role out, the Bath Indices were studied for reliability, speed, variability, reproducibility, and sensitivity to change. The studies involved a good sample size of between 163 and 392 subjects, some of whom were in-patients undergoing an intensive course of physiotherapy for 2 to 3 weeks at the RNHRD. The problem: The necessary limitations on clinical practice imposed by the COVID pandemic have meant almost all rheumatology appointments have switched to remote consultations. These consultations can be undertaken over the phone or via a number of different video conferencing applications. Soon into this switch, it was noted by specialist physiotherapists working in axial SpA that continuing to regularly measure BASMI was very challenging in these remote consultations. BASMI is generally considered a core part of regular review – most physiotherapists like to use it, but the real drive is from those people living with axial SpA who report it to be a great way to monitor their movements and how they are getting on with their exercises. Outcome measurements have been reported to: (1) Improve the quality of care (2) Improve patient-healthcare-professional communication (3) Tailor patient therapy to improve patient outcomes (Dobrozsi and Panepinto 2015) With no soon end to the restrictions to face-to-face appointments, there is a need to find a way to still work with people with axial SpA in this way. We are aware there are a number of projects on-going to develop digital methods of completing the BASMI and these are no doubt the future of remote BASMI, however, these could be a while yet in production and testing so we felt as a group that we HAD to come up with something to consider to use right now for remote BASMI assessment. Aim: To assess the feasibility and tolerability of a simple, immediately-available version of the BASMI for remote assessment and monitoring. Methods: The committee of the AStretch group of specialist physiotherapists reviewed the standardised BASMI instructions (https://nass.co.uk/wp-content/uploads/2018/09/Bath-Indices.pdf) and considered which components of the instructions would have to change to ensure they could be followed by the general public. Through the AStretch committee group, we drafted, re-drafted and eventually accepted a version 4 of the instructional document. For clarity and to differentiate this from the 1994 BASMI we have opted to name this re-draft home-BASMI (click here to access .pdf copy). To enable an assessment of the feasibility and reliability of this home-BASMI we identified the use of an upcoming online conference that included a number of specialist rheumatology physiotherapists and a large cohort of people with lived experience of AxSpA. With support from the National Axial Spondyloarthritis Society (NASS) we sent the home-BASMI document out, two weeks in advance, to the 97 booked attendees at this national axial SpA physiotherapy-themed conference - NASS-AStretch “Physio in Focus”. During this afternoon meeting we had two sessions where 7 physiotherapists were available in separate “tables” to assist people with axial SpA, and their helper in their household, to perform the BASMI according to our home-BASMI instruction sheet. In addition to the instruction sheet, potential participants were sent a cut-out-and-keep goniometer to assist in measuring the neck rotation; we requested that they supplied their own tape measure. We assessed how long it took to perform each set of measures and collected feedback from those being measured, their helper and the specialist physiotherapists guiding them.
 Results: As a part of the 7th Nov 2020 “Physio in Focus” meeting run jointly by NASS and AStretch, 21 people with a diagnosis of axial SpA were measured using home-BASMI, our novel remote, video-guided BASMI tool. There were 7 physiotherapists who assisted in the process of completing the home-BASMI measurements for these 21 people. All participants did have someone in their house to support them in undertaking the measures. The average time to complete the DIY-BASMI was 8 minutes. Feedback is as follows: Feedback from the people with an axial SpA diagnosis and their measurement helper | Positive | Mixed | Negative | “Easy to measure the side flexion, leg spread and tragus to wall parts” “Not complex to follow, the pictures helped a lot” “People have measured me before, but I’ve never been told why or what it means –thanks for letting me know today” “The handout provided a very helpful explanation and is an excellent facility” “Both the BASDAI and BASFI are self-report measurements. So get the BASMI out there for self-report.” “Making me think more about interpreting my measurements and using them gain more from my exercises.” | “I noticed a difference in my lumbar side flexion one side to the other – should I be concerned?” “could you produce a video of how to perform this?” “have trialled this week, but always get a different number for my forwards flexion” “the forwards lean feels the toughest to measure” “The spinal illustration measurement was the only one difficult to be reasonably precise.“ | “Where exactly is the tragus?” “Still not too sure where the L4 vertebra is” “The maths was a bit tricky” “have tried a few times, but always get a different number for forwards flexion test” “please create a video of this” “Courtesy of COVID it was not possible to ask another person in to help take measurements for myself. Not sure that I would want a friend or relative to do this anyway” “The back extension test (where you draw points on the lower back) was tricky - wasn't sure exactly where to put the points” |
Feedback from the physiotherapists | Positive | Mixed | Negative | “Not so tough as I had imagined” “Okay with BASMI naïve axial SpA – seemed okay to explain the how and why” “She hadn’t managed to print off the goniometer, I ‘eyeballed’ her Cx rotation, it was easy as she had 90o to one side and slightly less (roughly 85o) to the other” “brought in metal tape measures but managed to use with adjustments” “Less nerve-wracking than I expected…happy and confident at the end of the trial“ “patients were interested in what the BASMI means” “It seemed to go well and enjoyed by the participant” “I found giving clear instruction was key but honestly didn’t use a script as such as you want to keep observing and end up giving the instructions in mini-chunks as they get ready for each step.” “Making good use of the camera to demonstrate helped to…pointing to the tragus., demo of a chin-tuck etc.” “…had never had her measurements done before so had no prior experience. However, she found it straight forward and managed it really easily” | “you would need to have an engaged person who wants to be measured” “She did not have any previous experience of the BASMI…they were in fits of laughter doing the forwards flexion measure” “I think it's important to demonstrate no adverse events” “camera zoomed in would have identified measurement errors” “both felt sheets were helpful but required someone in person to go through the measurements too ”- felt explanations were helpful” “I think that the patients need to write the instructions with us and that we need to have several alternative ways which achieve roughly the same result remembering that this will be the way that they use each time.“ | “none were confident on finding L4 for the Schober's” “a video, as well as written instructions, might be helpful” “A video made will assist self-measuring at home” “A short training video may also help and we could ask the group if they wanted to see professionals or maybe more of a cartoon character or avatar image” “simplifying the maths would be helpful, especially in the lumbar side flexion protocol” “both female participants did not want to reveal their spine to the camera for LS flexion measures so unsure if they spotted L4 accurately” “measurement errors are definite” “only had a metal tape and therefore struggled with the schober measurement” “side flexion may be hard to stop people cheating if the person is really stiff” |
Limitations: These measures were not performed in a clinical setting and hence none of the data was shared. We are unable to assess how similar the results of this home-BASMI measurement technique would be to a traditional face-to-face BASMI. However, we had aimed to assess tolerability and feasibility. This was a very small sample size and a sample of convenience, all delegates had opted to book onto the conference and we would therefore assume that they would be more engaged with physiotherapy and its goals and purposes. Conclusion: There is sufficient feedback here to continue to the trial application of this remote consult version of the BASMI. It is not a perfect situation and we suspect the measures scored in this remote manner would struggle to show sufficient correlation to face-to-face to ever consider this as a valid, reliable replacement. However, in a situation where consultations are usually remote, we have shown the feasibility and tolerability of a remote-consult version of the BASMI. Future research: The long-term answer is almost certainly a digital assessment tool and we are delighted there is on-going research into this. We can however in the meantime recommend to fellow clinicians the remote home-BASMI protocol as a time-efficient and feasible option. Results from this version of the BASMI should not be compared to previous scores, but would still be a useful tool to allow reflection upon current exercise and stretch routines, to support self-management and to partially evidence any gross changes (negative or positive) in spinal movements. 
Authored by the whole AStretch Team
References: Calin A. Can we define the outcome of ankylosing spondylitis and the effect of physiotherapy management?/ Rheumatol 1994^1:184-5 Dobrozsi, Sarah & Panepinto, Julie. (2015). Patient-reported outcomes in clinical practice. Hematology. 2015. 501-506. 10.1182/asheducation-2015.1.501. Jenkinson TR, Mallorie PA, Whitelock HC, Kennedy LG, Garrett SL, Calin A. Defining spinal mobility inankylosing spondylitis (AS): The Bath AS MetrologyIndex (BASMI). J Rheumatol 1994^1:1694-8 Martindale JH, Sutton CJ, Goodacre, L (2012) An exploration of the inter- and intra-rater reliability of the Bath Ankylosing Spondylitis Metrology Index. Clin Rheumatol (2012) 31:1627–1631 Update for 2021...
WE WON AN AWARD!
A Turn for the Better
Having the chronic disease axial spondylathropathy (AS), has had its advantages. It has given me the opportunity to be part of a complex, evolving and fascinating world. Before my symptoms really kicked off whilst working in New Zealand, I was destined to follow a long career in general outpatient physiotherapy. Now looking back, however, I had rather fallen into rather than chosen this path. In 1992, following my spell recuperating from reactive arthritis (see previous blog for more information) and under the expert care of Dr Ian Gaywood at Swindon Hospital, my journey began. My role as metrologist soon expanded into clinic work encompassing all aspects of patient care and assessment. At a time when outcome measures were not yet standardised, I then joined Dr Calin and his team at ‘The Min’ in Bath interviewing patients in preparation for the Bath indices. These were exciting times
 Subsequently, I heard about the inspirational work of physiotherapist, Sue Fletcher, and her team of Allied Health Professionals (who were mainly Physiotherapists) at Christchurch Hospital. As part of her dedicated rheumatology follow-up clinic, I continued to be mentored as I learnt to decipher blood results and X-rays, and advise patients on their (rather limited at that time) medication. We were shown how to inject shoulders, wrists and knees. We were ahead of our time but few people knew of our existence. In 1994, acknowledging the need for more formal training, the whole team were encouraged to undertake a specially devised Post Graduate Diploma and Masters course in Advanced Clinical Rheumatology at Bournemouth University. This comprehensive 2 year course was compiled by Sue Fletcher and Dr Karen Mounce, Consultant Rheumatologist at Christchurch Hospital. Once graduated and buoyed up with enthusiasm, we decided to call ourselves Rheumatology Practitioners. We thought that as an army of practitioners we were going to conquer the world!! Sadly this was not to be the case. After we had graduated, the University course was never repeated and that is a great loss. The course relied on undergraduates being part-funded by their hospital but at the time, few hospitals shared our enthusiasm or had the funding. However, armed with the skills and confidence, I decided to start up more rheumatology follow-up clinics closer to home. Despite being a Physiotherapist and not a Nurse (who traditionally took these roles), I managed to convince the medical staff at both Salisbury and Southampton hospitals that they needed me as a side kick to lessen their load and that I was also good value for money! The Consultants were extremely trusting and supportive in my work with the patients and they had an open door policy in times of need. Patients were happy to be seen by someone who could empathise with their symptoms, was at the end of the phone in times of need and could offer them the time they needed in clinic. We were still pre-biologic therapy at this point so care needs were complex and drug side-effects were a constant issue. Salisbury and Southampton had an excellent Physiotherapy and Occupational Therapy department and all my patients spent time in these departments as part of their programme. Although I was not working as a traditional Physiotherapist, my previous experience in MSK came in useful and with the support of NASS, I over saw the creation of the Southampton and Salisbury NASS exercise groups.
Then, the late, great, Physiotherapist, Jane Barefoot nominated me as Physiotherapy Advisor to NASS; but walking in her footsteps proved to be a difficult task. I felt I could not carry the burden alone and that patients so desperately needed more help. A group of rheumatology physiotherapists heard my cry for help and AStretch was born in 2001. The not-for-profit organisation has subsequently grown into to what it is today making a huge impact in patient care and knowledge dissemination. Meanwhile I continued my work as Rheumatology Practitioner and I really felt that I had found my calling. For nearly a decade, I enjoyed helping to solve complex issues, gaining knowledge and making good friendships with the patients and staff. When I left work in 2004 to look after my young daughter, biologics were in their infancy and life for the staff and patients were about to change radically. Sadly it took many more years before AS patients could benefit from Biologic therapy but I can talk from experience, it has been a life saver. Nowadays there is so much more help, support and guidance for patients with AS. NASS now employs 10 staff and amongst many other initiatives, is involved with parliamentary campaigns to increase the profile of AS and AStretch is an integral part of the organisation. In hospital departments across the land, rheumatology is taking centre stage and there are Allied Health Professionals working as clinical specialists making a big difference. Many of the frontline staff are members of AStretch and many have contributed by attending AStretch courses and conferences. As a member of AStretch, I feel privileged to be working alongside physiotherapy colleagues so passionate about the care and wellbeing of AS patients and their families. It has been so rewarding and such a pleasure to be part of this world and I consider myself lucky as my career would never have gone in this direction without my AS.

Juliette
Outcome Measures2018: The Bath Indices, outcome measure information booklet, for use with A.S. patients, was reviewed and edited by four members of the AStretch Committee- Heather Harrison, Karen Irons, Amanda Thomas and Jane Martindale. The extensive reference section represents the vast literature search undertaken, this was supported by the librarians at Wrightington Wigan and Leigh NHS Foundation trust. 
|