Service Development and Advancing Practice blogsWe all have a responsibility to ensure we are delivering best-practice in our clinical roles. These blog entries aim to share service development ideas to support the physiotherapist working with and for people living with axial SpA / AS. We also want to highlight the emerging advanced practice and extended roles of physiotherapists and other members of the multi-disciplinary team in supporting axial SpA / AS services. Key Documents
 More to follow here...
Our Aspiring to Excellence Journey
Maureen Motion, Extended Scope Physiotherapist Rheumatology, based at Freeman Hospitals, Newcastle Hospitals NHS Foundation Trust. Our team, led by Dr Lesley Kay and Dr Ben Thompson applied to be part of the First cohort of Aspiring to Excellence in July 2019. Aspiring to Excellence (A2E) is a strategic partnership between NASS, BRITSpA and sponsoring companies AbbVie, Biogen, Lilly, Novartis and UCB. It is an award programme designed to encourage and recognise service improvement in Axial SpA care, helping to reduce the delay to diagnosis. The programme aims to provide comprehensive support to selected rheumatology teams to help them with improvements within their departments, with the expert help of the NHS Transformation Unit.  Aspiring to Excellence Quality framework- we initially had to describe and rate our service and the current processes that we had in place around 10 statement headings including areas like: · recognition and referral · diagnosis in specialist care settings · information and support that we provide our patients with · pharmacological support and non-pharmacological support of axial spondyloarthritis · flare management · our support for long-term complication · how we address mental health and emotional wellbeing of her patients This process gave us the opportunity to really look at what we provide as often when we are all very busy, chasing our tails in hectic clinics it is easy to forget and overlook the excellent aspects of care that we provide and sometimes only see the negatives. Our application was short listed and we were invited to an interview on Monday the 4th November 2019 at 1:00 a.m. lasting 45 minutes at the Royal College of Physicians in London, which in itself seemed a daunting experience. The lead consultants Dr Lesley Kay and Dr Ben Thompson, Michelle Rutherford, specialist nurse and myself all attended the interview, where we had to present a 10 minute presentation outlining three areas of our service that we would like to improve. We decided to concentrate on 1. Reducing referral delay and extending our specialist Axial SpA ‘self-referral, self-management’ programme into the community. Our musculoskeletal services had just been decommissioned and the tender awarded to an NHS organisation called Tyneside Integrated Musculoskeletal Services (TIMS) that were incorporating primary and secondary care physiotherapy work across the Newcastle and Gateshead areas. 2. Improving overall health for patients with Axial SpA by implementing ‘annual review.’ 3. Making the best use of our department service by reviewing the way we deliver services and investigating innovative ways of working. Walking into the interview room, we were met with a sea of faces, patient representatives, NASS personnel and AStretch representatives sat round a large table. The interview seemed to pass very quickly, all of us though given the chance to speak and answer questions. On 16 November at the NASS Voices event in London where it was formally announced which services have been awarded a place on the programme, we learned of our success. As a department we were so pleased to have been offered a place on this prestigious programme but also appreciated that there would be a lot of hard work involved over the next 3 years.
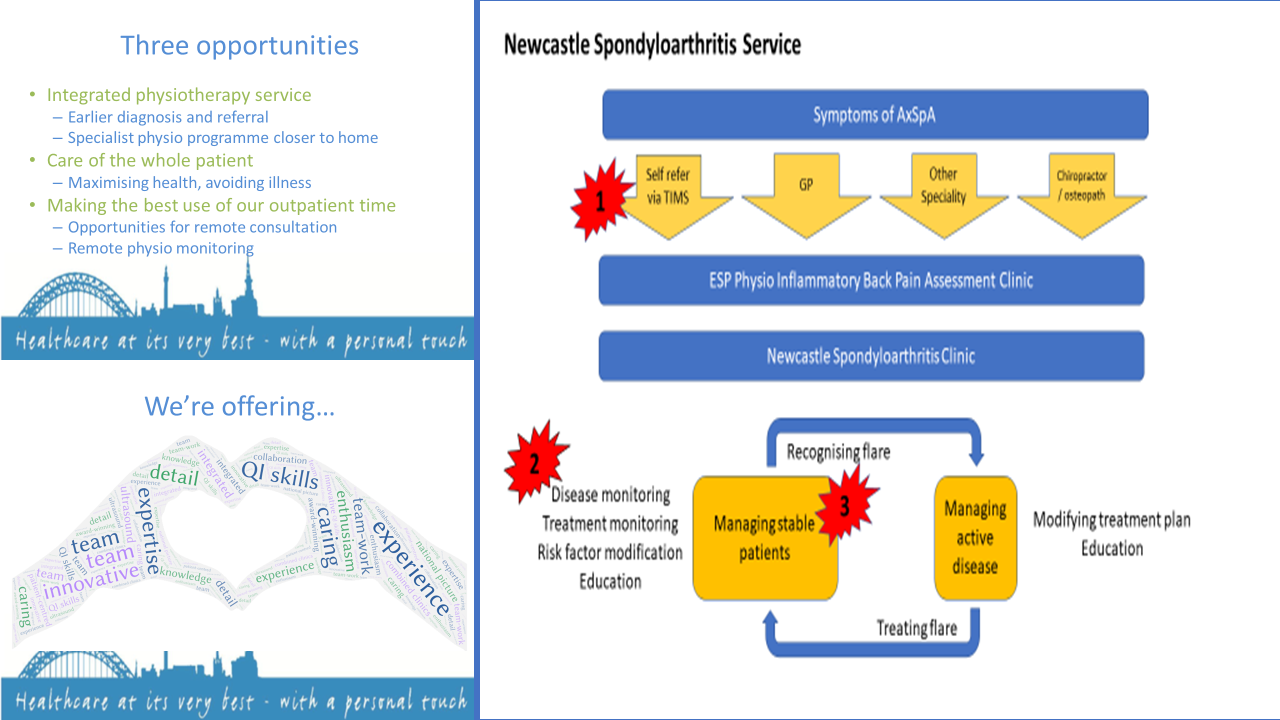 Tuesday 3rd December 2019 from 10.00am–4.00pm - we were invited to the first learning event to meet the NHS Transformation Team, Dale Webb CEO of NASS and the other teams on the programme. The programme for the year was out lined and we were to attend as a team for 7 dates throughout 2020. We came away from the 1st day totally inspired, full of motivation and team spirit of how we could really make a difference to our patients with the help of this programme. We were also given the opportunity to get some team time away from the pressures of a busy department which was invaluable. We much appreciated the opportunity to network with other teams and hear about their improvement projects and challenges. This early face to face team work allowed us to dedicate time to Axial SpA service development, to focus our goals, to leave the hospital environment and network and to learn from other teams. We decided that we needed more details and data from our current service from initial referral to diagnosis and to map out a number of actual patient journeys, looking for any bottlenecks and areas where there were potential time delays to diagnosis. Two weeks before we travelled to Manchester I had unfortunately fallen off my bike and sustained a fracture to the greater tubercle in my shoulder. I was unable to do clinical work but this gave me ample opportunity and time to complete this initial stage of our project. Ironically, this was pre-COVID where video attend anywhere and telephone calls were virtually unheard of as a means of assessing patients! We also used this time to make contact with our key stakeholders and management that we would need to work with in order for the project to be successful. We also fully engaged the rest of our Axial SpA team who didn’t attend the interview process- Occupational therapist Gemma O’Callaghan, specialist Nurse Lesley Tiffin, and Consultant Rheumatologist Dr. Rachel Duncan. Our next A2E day was 12 March 2020 in Manchester- little did we know that 11 days later, the lockdown would start and that would be our last in person day! Hopefully we can all attend the Celebration, end of programme event in June 2022. We managed to keep working on our projects over the next year, obviously dipping in and out, as many of us were re-deployed to different COVID roles. From these first 2 sessions we compiled driver diagrams and started PDSA (plan-do-study-act) cycles to effectively implement QI. The patient journey was mapped, identifying the referral source of patients with suspected Axial SpA. Training of community based physiotherapists in the TIMS organisation was then implemented, including briefing on the importance of identifying Axial SpA and recommended use of screening criteria - specifically, the Assessment of Spondyloarthritis International Society (ASAS) Expert Criteria for Inflammatory Back Pain Assessment. The quality of referral from TIMS was assessed, exploring use of ASAS expert criteria. Delays in time from referral to 1st appointment in the Extended Scope Physiotherapist inflammatory back pain screening clinic were assessed. In December 2020 we had an online event where we presented our improvements and inevitable challenges over the 1st year of the programme. The NHS Transformation Team did a fantastic job of keeping us motivated and trying to concentrate on the small gains that we have made despite very challenging circumstances.
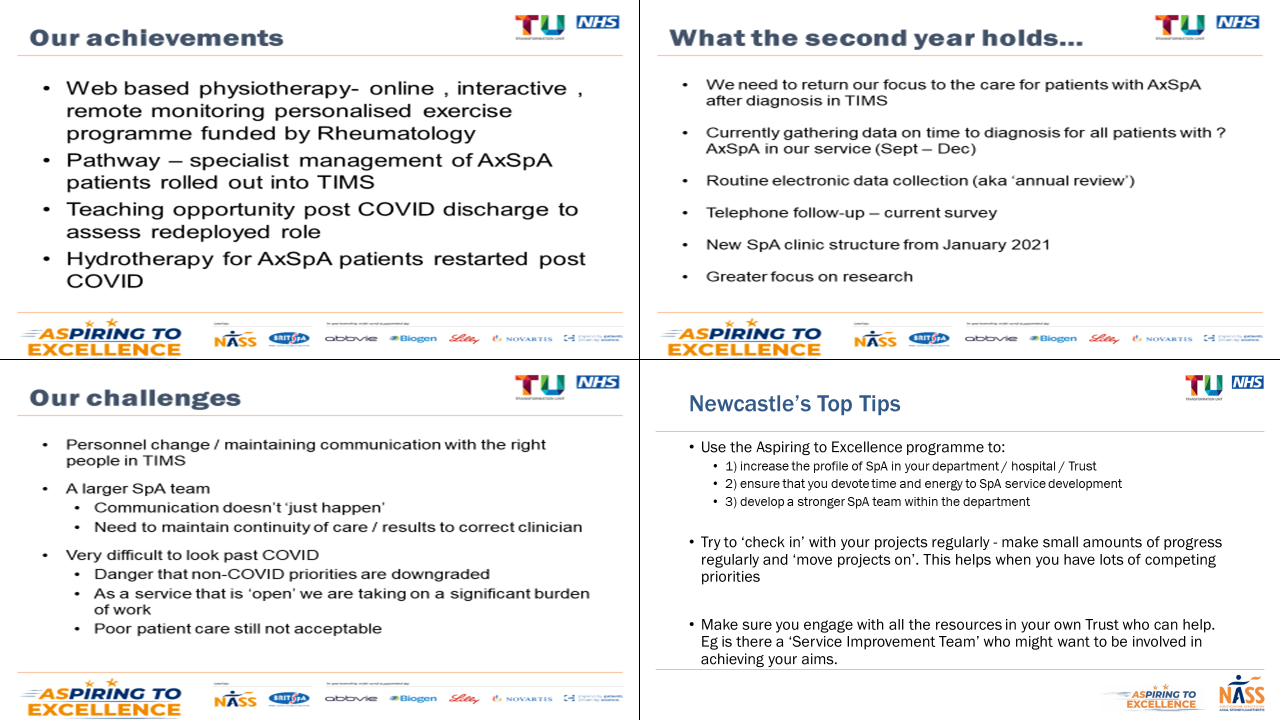 On reflection, being part of A2E, I feel gave us the catalyst and enabled us post COVID to kick-start our services and we also had the drive and motivation of the NHS Transformation Team. At end of year one, around our 2nd aim, an electronic annual review sheet was developed, (by new consultant rheumatologist Dr Ejaz Pathan), to be included on the electronic record with collated information on co-morbidities and additional health checks. Innovative ways of working were re-explored, including a hybrid/virtual/in-person model of care and use of the ePROMs - the process much accelerated as an inevitable response to the pandemic. Our 3rd aim was around innovative ways of working. We embedded a Web-based programme called Giraffe Health care www.giraffe.com into our Axial SpA management, a platform for the delivery of personalised physiotherapy programmes. Throughout 2021 we worked on our improvement areas and were kept continually motivated by the NHS Transformation Team- coaching sessions, networking days, and the last session in February 2022 was dedicated to individual teams ,having uninterrupted time to work on their projects. So what have we gained through A2E? Has it been worthwhile? We have learnt lots through this process. Driver diagrams in particular have been really helpful to contemplate and write down; they will permeate the way that we work throughout the rest of our careers, and we will use the more formal structure where it is helpful. But also, just to realise that the way to get things done within the NHS is to demonstrate the change, that story that you tell, that you say this is what we tried to do, this is what we measured at the beginning, this is what it was like then, these are the steps that we took, and this is what is different now. 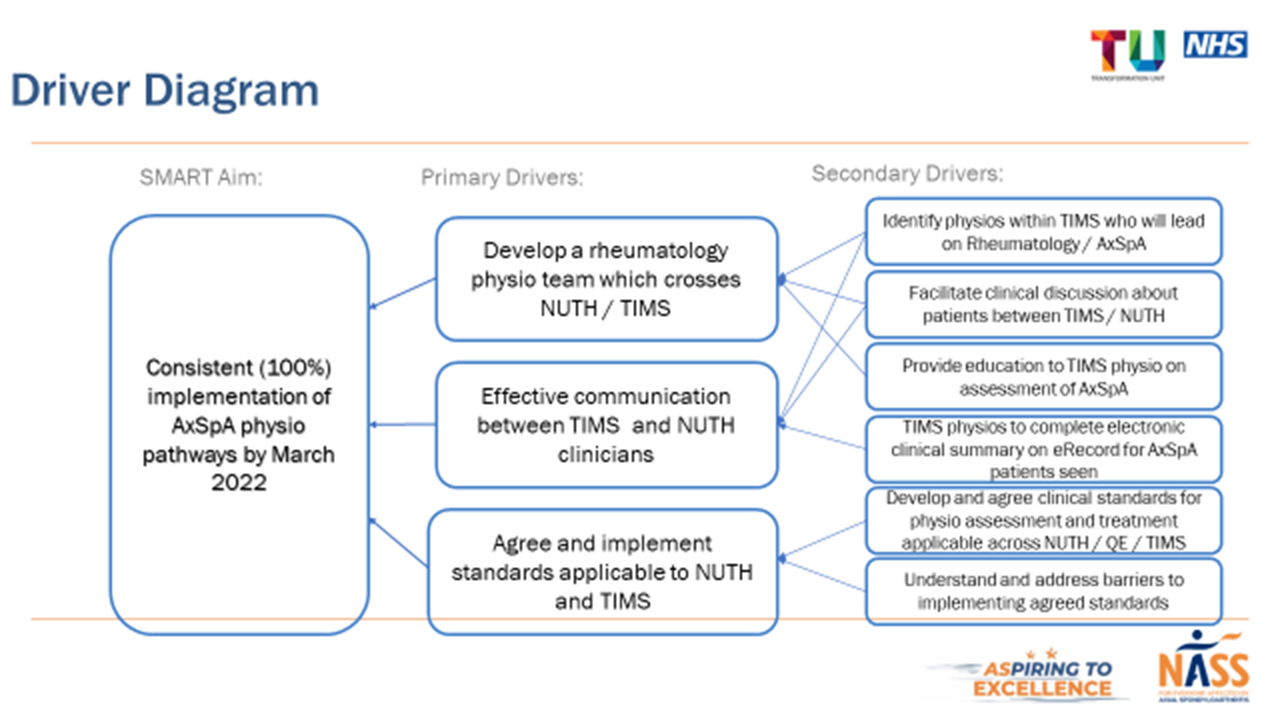 It has been great to see what other teams on A2E have managed to achieve, and also to reassure you that no one’s finding it easy, and no one does it in a simple and straightforward way, which motivates you to carry on striving to make those changes.
Personally, A2E has been a fantastic CPD opportunity, and has greatly improved the service that we offer our patients in Newcastle. We have strong, evidence-based pathways in place now. I would encourage any Rheumatology team to strongly consider applying to join the A2E programme- we have gained so much. And the programme is still ongoing. 
Mo
A Physiotherapy Response to the BSR "Rheumatology Workforce" Report
July 2021: The British Society of Rheumatology have recently released a “Workforce Report”, it includes exciting potential developments for all of the multidisciplinary team. This BSR document talks about "enhancing roles" for the AHP workforce in rheumatology and clearly these "enhanced roles" speak to the advancing practice agenda coming from other areas of the National Health Service. There have been developments elsewhere with regards to advancing practice, for instance, the Centre for Advanced Practice that Health Education England have just launched; and hopefully similar advanced practise support will very soon follow across the other three nations that make up the UK.
When we think of advanced practice historically, perhaps we think of band 8 roles, but now we're seeing advanced practice roles advertised at band 7 level, maybe to better match the banding amongst nursing staff. We do also have to be aware of independent providers of rheumatology services who will also offer advanced practice rheumatology physiotherapy roles, but outside of the NHS agenda for change banding structure.
The BSR document suggests that bands 6,7 and 8 should be looked at and, in their phraseology, “enhanced” to allow allied health professionals to meet the increasing demands across healthcare services in rheumatology. This report, taking information from GIRFT, NEIAA and member engagement, does accept that there are quite wide variations in the application of AHP roles across rheumatology. These findings are in keeping with the national rheumatology physiotherapy survey undertaken October 2019 and quite recently published: we described 40 different roles a physiotherapist might undertake in rheumatology, and there were varying scores of applications of those roles across different banding levels, as well as across different parts of the country. We do hope with the very imminent release of the Rheumatology Physiotherapy Capabilities Framework there will be a chance to better balance the way rheumatology physiotherapy roles are provided. In balancing these roles, there is also a fantastic opportunity to enhance and advance what is undertaken by us as rheumatology physiotherapists and what we can offer to the rheumatology team in these times of increased demand and other challenges related to the peri-COVID and, hopefully soon to come, post-COVID environment. Data presented in the BSR report, picked from the NEIAA, shows that 50% of UK departments do not have a physiotherapist embedded in their MDT. More concerningly, 7% of Trusts reported that they didn’t have access to physiotherapy services. The BSR report shares some information from the yet-to-be-released GIRFT report on rheumatology, it states that GIRFT “found that departments in England were not making best use of the multidisciplinary skills mix of the team, and that this could be harnessed to address capacity challenges, optimise services and increase their resilience and sustainability”. Whilst accepting there is no such thing as a typical MDT; the BSR report does present data for an “average UK rheumatology department”. This shows the current average of 1 whole-time equivalent rheumatology physiotherapist for every 5 and a quarter rheumatology consultants. Or for every full-time rheumatologist, you would require about 1 day per week (7.5 hours) of rheumatology physiotherapy to match the current national average. Finally, in considering service demands, waiting times and health outcome improvement, the report gives a suggestion/recommendation of one rheumatologist per 60-80k population. It can be extrapolated from these numbers that recommendation could be one rheumatology physiotherapist per 315-420k population. The penultimate paragraph of this blog and really our call to action as members of the rheumatology MDT, must come verbatim from the BSR report… “BSR is calling for Trusts and Health Boards to establish more enhanced roles for AHPs, pharmacists and nurses within rheumatology departments. Departments should be open to reviewing who does what within their team and whether there are better ways to make use of the multidisciplinary skill mix of the MDT. Staff should be encouraged to develop their specialist skills and extend their scope of practice with departments providing the opportunities to do so. These roles must be recognised with appropriate Agenda for Change (AfC) banding in line with the specialist skills required and to ensure that they attract qualified candidates” So, whether you still use the term "extend their scope" or if you would rather be "advancing", now is the time to take this BSR workforce report (and perhaps some of your local data) to your managers, your rheumatology colleagues and whoever needs to hear this message. Physiotherapists can and will adapt and progress to meet the challenges in the rheumatology workforce.
References
BSR (2021) Rheumatology Workforce: a crisis in numbers
https://www.rheumatology.org.uk/Portals/0/Documents/Policy/Reports/BSR-workforce-report-crisis-numbers.pdf?ver=2021-06-16-165001-470
Gregory WJ, Burchett S, McCrum C (2021) National Survey of the Current Clinical Practices of UK Rheumatology Physiotherapists. Musculoskeletal Care 19:136–141.
https://onlinelibrary.wiley.com/doi/epdf/10.1002/msc.1516
Gregory WJ, McCall GJ, Shaw K, Martindale J, (2017) BENCHMARKING THE NORTH-WEST SPONDYLOARTHRITIS PHYSIOTHERAPY SERVICES, Rheumatology, Volume 56, Issue suppl_2, April 2017, kex063.002https://doi.org/10.1093/rheumatology/kex063.002

Will
Setting up an Axial SpA / AS clinic
July 2020: Our May 2019 blog memorably described Juliette’s experience in the early-to-mid 1990s in setting up clinics for people with Ankylosing Spondylitis and the side-by-side work of developing the Bath scores (https://secure. toolkitfiles.co.uk/clients/23905/sitedata/Blogs_and_own_content/A-turn-for-the-better.pdf). Since this time the Bath scores have become gold standard; but, we ask has the practice of having a physio in your axSpA clinic also become so well established?
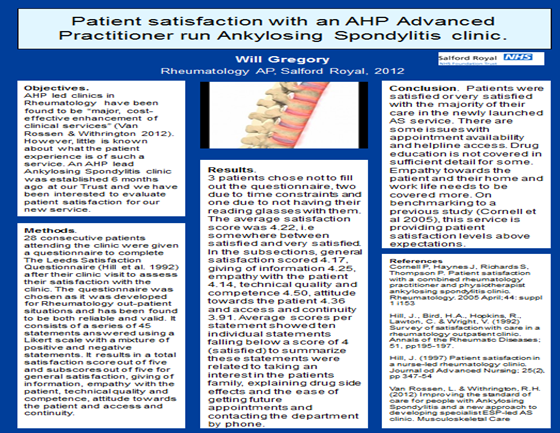
Approximately a decade ago physio-led AS clinics began to be established in the UK. The first example published, described this new approach to AS management by means of developing specialist extended scope practitioner led AS clinics (van Rossen, 2012). The question now to ask is what have we learned since this time? More pertinently, especially in this unprecedented COVID-19 era, we now need to think about how the provision of this kind of a service has developed and how it can be taken forward?

Here at AStretch we do continue to get queries from physiotherapists who are keen to set up a service in their Trust. Whilst there has not been rapid, national adoption of AHP extended scope (or more recently advanced practice) led clinics, there has been a gradual change towards AS specific clinics and the physiotherapist is often at the forefront of such services. This is an area of development that has been shown to improve patient care and patient satisfaction (Cornell, 2005; van Rossen, 2012; Adshead, 2019). This blog is our first step in attempting to share the knowledge and expertise of experienced clinicians in the “how to” of establishing an axSpA clinic.
Unfortunately, this is a not a ‘one-size-fits-all’ scenario, hence we plan in this blog and future editions to share some reports from exemplar services. The 2020 NASS led national enquiry of English axSpA services is telling, and its’ recent nationwide review is pertinent to why we feel further explanation of the clinic role is now needed (https://nass.co.uk/wp-content/uploads/2020/01/Axial-Spondyloarthritis-Services-in-England-FINAL.pdf). More importantly we need to adjust our thinking as a consequence of the impositions from COVID-19 where the ‘new norm’ is transforming from traditional ‘face to face’ contact. Consequently, we need to think towards adoption of the ‘virtual world’ with regards to patient consultation models as a rheumatology physiotherapy professional subgroup when considering how we can best serve our axSpA patients. Crucially, the patient is the lead in these changes, we give examples where patient and public involvement in service developments has been a key component and we also have updates on patient satisfaction and further stakeholder review for more established axSpA clinics. Historically, in the care of people with AS, there is some evidence of the benefit of physiotherapy involvement in rheumatology clinics (Cornell, 2005,) and in physiotherapy led clinics (van Rossen, 2012, Moran, 2016). One of the most successful implementation benefits from physio-led axSpA clinics have been recently further demonstrated (Adshead, 2019). This service, in London, was established by Rebecca Adshead and colleagues in 2010, and has consistently been shown to quite remarkably decrease the delay to diagnosis of axSpA. In fact since the introduction of this service it has been shown to reduce the delay to diagnosis from 8.5 years to approximately 3 years (Adshead, 2019). Nationally, however the challenge of the extent of unrecognised axSpA of patients referred to, and missed in, musculoskeletal clinical practice continues to exist (McCrum, 2020). The challenge remains to raise expertise and confidence within primary care teams to screen for and recognise inflammatory back pain and to refer onwards. If that referral onwards could be made to physiotherapy led clinics, akin to the model described by Rebecca Adshead and colleagues, the potential benefit for patients would be obvious. As we warned, there is no one size to fit all but we include personal stories of examples of setting up an axSpA clinic can be achieved.
Example 1
Will Gregory, Consultant Physiotherapist (Rheumatology), Salford Royal NHS Foundation Trust
For the first year or so I did have a Consultant Rheumatologist next door to assist me; but I have always been seeing the patients instead of, rather than in addition to the Consultant or Registrar’s review. Clinical validity of this service is evidenced elsewhere, but for our managers and the business case we wrote we focused on the advantage of freeing up the medics by having the physiotherapist completing the reviews at months 6, 12 and 18 months of a 2 year cycle (with Consultant review at month 0 / 24) . On a personal basis, this continuity of input has allowed me to build up a good working relationship with this cohort of patients and the outcomes of better exercise / active lifestyle compliance are clear. The need for regular review of patients (3 monthly initially in the early 2010s, now 6 monthly) who receive biologic medication had added unnecessary ‘extra load’ on the medical team. Whereas in a physiotherapy led clinic, the frequency of review seemed more relevant to allow close monitoring of BASMI and adjustments of home and gym-based exercise programmes accordingly. Patient satisfaction in the physio-led clinic was very good (we used the Leeds Satisfaction Questionnaire to assess this) and is demonstrated in this poster (shared in case you want to replicate in your axSpA physio service!):
It has not been plain sailing since set up in 2011 and we have had to adapt the clinic to a number of issues. Firstly, was the NICE guidance to drop from 3 to 6 monthly assessments of biologics responsiveness. The consequence of this was that it enabled us to reduce follow up frequency and ‘open up’ the clinic to more patients. We then embraced the ‘virtual world’ and had a battle with the Informatics Department to attempt to be able to develop and implement an online Bath questionnaire collection resource. However, this proved to be ‘non-fruitful’ and we have had to remain paper based for our outcome measures (but we eagerly anticipate the BSR ePROM project going live!). I work with 10 excellent and amazing rheumatology consultants, somewhat understandably they all want to maintain an interest / specialism in axSpA; for that reason we do not have a named clinical lead for our axSpA service. The physio-led part of our axSpA service allows equity of provision for people with axSpA under the care of anyone in our team. Research has shown that BASMI scores have much better intra-rater than inter-rater reliability (Martindale 2012) and hence the ability to have one person measuring these over time allows a more accurate assessment. Crucially, the physiotherapist measuring BASMI directly ties into HEP adaptation where scores are showing big changes and also facilitates discussions about any improvements and benefits seen, linking the benefits into good exercise habits and practices. We’ve had a couple of formal service user / PPI meetings in our AS service over this period. We have been keen at these open forums, as well as many other informal occasions, to get the users (patients) opinion of how the service is working. Process mapping on these meetings has allowed us to discover bottlenecks and inefficiencies in the patient journey. We’ve changed our communications on appointments, as well as attempting to change the way we collect outcome measures and the steps taken on a typical clinic visit. The clinic continues to provide 6 slots per week which enable all patients who choose the physio-led model to access it. The majority of our axSpA cohort have chosen to access the clinic, but a few have remained loyal to their rheumatology nurse. Some have opted for the less frequent review by their Consultant Rheumatologist, but most are happy with a mixture of clinicians performing their reviews. Whilst patients on biologic medication make up the majority of the clinical cohort, since the NICE shift from 3 to 6 monthly review of biologics, there is availability to review those who take only NSAIDS or indeed have the good fortune to be able to control their symptoms by exercise alone. The clinic is also open for new patient referrals to access ‘work up’ to diagnosis. However, until recent changes most patients will have had a diagnosis prior to choosing the service, or perhaps be awaiting their MRI scan results and be aware of the potential for a differential diagnosis. The term ‘annual review’ has become more of a buzz word since this clinic was established. We have ensured that our service as a whole encompasses all the review areas recommended within NICE guidance. However, formal implementation of each and every component within the annual review is difficult within one session and consequently our current service has adopted a shared application of this which takes place in both the the consultant-led review and the physio-led axSpA clinic. Running the axSpA clinic ties in very nicely with also running the regular gym and hydrotherapy AS exercise sessions. I’m very fortunate to have a rheumatology physio team around me and hence these days I only make the first hour or so of our exercise session – this allows me to catch up with our regulars, to welcome new starters and, perhaps most importantly, to build a bridge between our rehabilitation and assessment / review services for our people with axSpA. It also means both this great group of people with axSpA and I get to pass on our experience and enthusiasm for axSpA exercise treatment to all the physios and therapy assistants who rotate through our rehabilitation service. Example 2
Heather Harrison, Specialist Rheumatology Physiotherapist, York Teaching Hospital The physio-led clinic in York is set up to see patients on an annual basis. There is a mixture of patients on biologics and those who manage with NSAIDs and other therapies. The clinic is called an Inflammatory Back Pain Clinic and also sees patients with psoriatic arthritis, if they have a predominantly spinal disease and patients who have inflammatory bowel related disease. Patients on biologics see the consultant at alternate 6 months. The Bath Indices are completed and advice and education given. The clinic runs at the same time as other consultant clinics so if a steroid injection is required it can be prescribed. The clinic runs every 2 weeks and provides 6 slots. The idea is that all patients with Inflammatory Back Pain would attend this clinic so they have metrology completed and physiotherapy input annually. Example 3
Claire Jeffries, Physiotherapy Clinical Specialist in Hydrotherapy and Rheumatology for Solent NHS Trust Here follows an example of clinic set up from our service. Please do send us your examples to add to this resource. There will be many different ways of running axSpA physio clinics and we’re keen to collect information on the breadth of services across the UK:
Approximate service population: 600,000 | Clinic | Staffing | Frequency | Patients per clinic | Time per patient | Additional points | AS Annual review | Physio (B8a) | X 2 a month | 6 | 45 minutes | Patient is also seen annually by Consultant (appts consultant – physio at 6 month intervals) | NB – patients can move between clinics according to planned care as clinical required | AS biologic - screening and review | Physio (B8a) CNS (B6) | X 4 a month | 4 - 6 | Screening = 1.5 hrs Review = 45 mins | CNS and Physio have level of interchangeable roles to accommodate for leave / sickness and therefore for clinic to continue with one member of staff | | Biologic patient pathway*: Year 1 : Screening, week 12 or 16, 12 weekly thereafter Year 2 : 6 monthly between CNS/physio clinic & consultant *adhoc clinic appt is available if patient deteriorating or requiring review |
Roles you might perform in the clinic- Before seeing the patients review their medical history, previous consultations, and previous physiotherapy and pharmacological treatments.
- Liaise with appropriate Rheumatologist prior to seeing patient to clarify any issues
- Explain the risks and benefits of treatment options in ways that can be easily understood
- Offer verbal and written communication to allow patients to better understand their diagnosis and it's management
- Objective assessment according to BASMI
- Objective assessment according to PsARC criteria
- Assess for need for physiotherapy, hydrotherapy, podiatry, occupational therapy, joint or soft tissue injection
- Consider offering short-term treatment with glucocorticoids (intramuscular or intra-articular) to rapidly improve symptoms.
- Use non-medical prescribing training to suggest prescriptions
- In people with established axSpA whose disease is stable, cautiously reduce dosages of disease-modifying or biological drugs.
- Offer analgesics (for example, paracetamol, codeine or compound analgesics) to people whose pain control is not adequate and is thought derive from non-inflammatory processes
- Prescribe and teach exercises for enhancing joint flexibility, muscle strength and managing other functional impairments. Provide written instruction including diagrammes for these exercises
- Medication review
- Assess the need for referral for orthopaedic surgery
- Biologics review - as per NICE guidance and departmental guidance
- Request bloods to monitor disease status, if appropriate (60% of axSpA patients don’t show active disease on ESR or CRP)
- To order immunological tests to review diagnostic states
- Request x-rays, ultrasound scans, MR scans, nerve conduction tests, guided injections, DEXA scans
- Measure for, order, and provide orthotics devices - walking stick, crutches, frames, basic hand splints, braces for knees, elbows, etc. Refer to orthotics assessments for more detailed / complex needs
- Book follow up appointments in hydrotherapy and physiotherapy; request follow up appointments within Rheumatology
- Liaise with other members of the team to get best results
- Dictate clinic letters according to departmental "gold standards"
- Update clinical diagnosis on relevant statistical collection platforms - EPR, biologics registers, Blueteq, departmental data list
- Discuss, offer and recruit participants into going local, regional and national research studies
- Dictate letters to other clinicians to instigate assessment and treatments as indicated
- Dictate letters to other agencies as requested by patients / indicated eg. discounted gym membership, occupational health departments about return to work guidance, benefits departments
- Feedback to patients (as appropriate) their results of x-rays, MR scans and ultrasound investigations and the implications of these findings to their ongoing care
- Re-enforce messages about given diagnoses and aid in patients coming to terms with this and accepting recommended treatments from the team
- Discuss return to work issues where relevant
- Inform patients of other relevant services; eg. self-help groups, community exercise programmes, national centres of excellence
- Provide educational experiences and relevance for observing medical students, visiting GPs, other students
- Liaise with the patients family in an appropriate way for their needs, the patients’ needs and to facilitate better treatment adherence
- Aid other members of the team in their consultations as indicated.
- Provide timely appropriate on the spot physiotherapy advice and treatments.
And that is where we have got to in a few frantic weeks of trying to respond to our most recent query on setting up an AS / axSpA physio clinic. We do hope this has been helpful, but appreciate this blog doesn't flow fantastically, but it does at least show how we all do things slightly differently - and does mean a variety of resources to be used by those trying to set up their own clinics.
 |
|
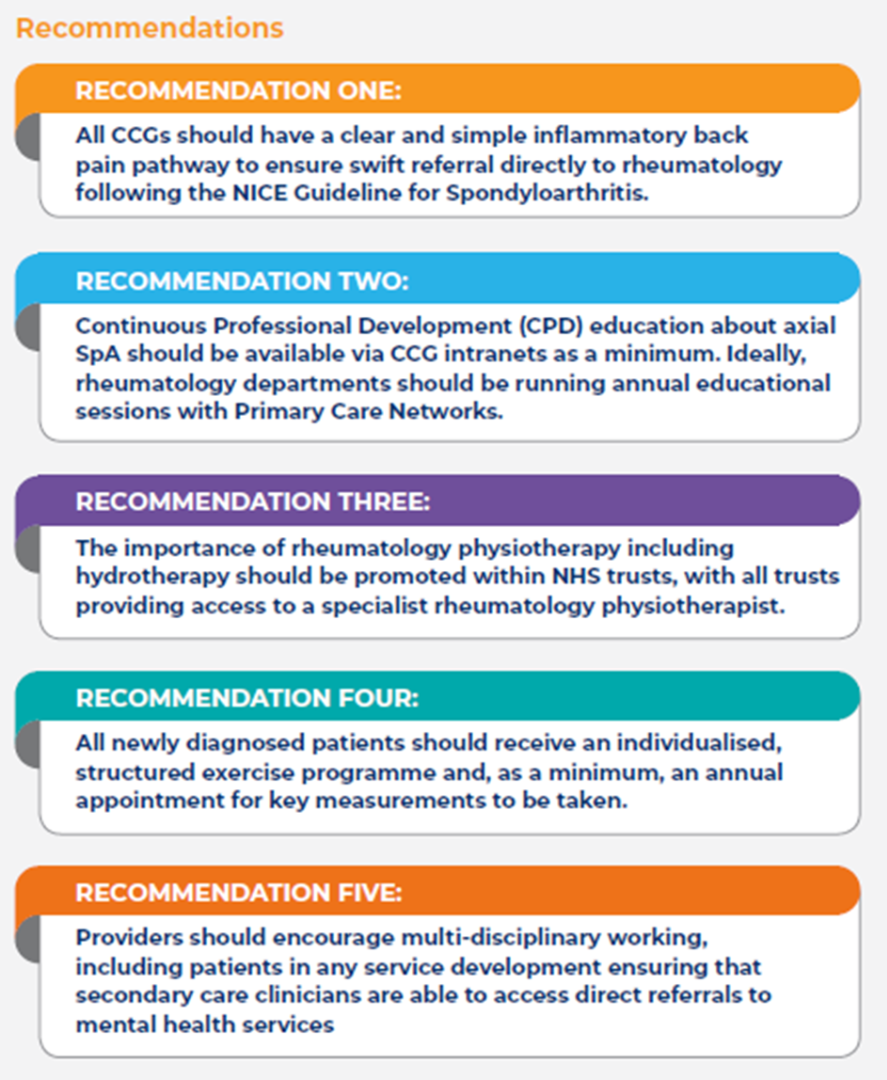
^^ Recommendations from the NASS (2020) document “Axial Spondyloarthritis services in England A NATIONAL INQUIRY”
Publication on this website is not a one-way street, we can work this information up over the coming weeks / months into a more comprehensive resource - please do consider this a "road test". It is also part one of a series, so if you would like to feature your AS / axSpA physio clinic please do get in touch comms@astretch.co.uk, we would love to feature your work and experiences!
 Will Will  Jane Jane  Heather Heather  Claire Claire
References Adshead R, Tahir H, Knight P, Donnelly S (2019) Oral Presentation OP0002 EARLY INFLAMMATORY BACK PAIN SERVICE – REDUCING TIME TO DIAGNOSIS IN PATIENTS WITH AXIAL SPONDYLOARTHRITIS – THE FIRST 8 YEARS Annals of the Rheumatic Diseases 2019;78:66-67. https://ard.bmj.com/content/78/Suppl_2/66.2.abstract Cornell P, Haynes J, Richards S, Thompson P. Patient satisfaction with a combined rheumatology practitioner and physiotherapist ankylosing spondylitis clinic. Rheumatology. 2005 April;44: suppl 1 i153 McCrum C, Kenyon K, Cleaton J, O21 Unrecognised inflammatory back pain: a retrospective review of people presenting to musculoskeletal physiotherapy with undiagnosed axSpA, Rheumatology, Volume 59, Issue Supplement_2, April 2020, keaa110.020, https://doi.org/10.1093/rheumatology/keaa110.020 Martindale JH, Sutton CJ, Goodacre, L (2012) An exploration of the inter- and intra-rater reliability of the Bath Ankylosing Spondylitis Metrology Index. Clin Rheumatol (2012) 31:1627–1631 Moran S, Longton C, Bukhari M, Ottewell, L. AB0708 Delay To Diagnosis in Ankylosing Spondylitis: A Local Perspective Annals of the Rheumatic Diseases 2016;75:1146-1147 Van Rossen L, Withrington R.H. (2010) Improving the standard of care for people with Ankylosing Spondylitis and a new approach to developing specialist ESP-led AS clinic. Musculoskeletal Care 10: 171-77 https://onlinelibrary.wiley.com/doi/full/10.1002/msc.1015
Tap, Tap…What’s App?
 February 2020: Firstly, I must apologise for my attempt to bring the classic ‘Knock Knock’ humour of my past into your digital present. I suspect it has not worked. However, it has introduced the topic of Digital Health in Rheumatology for this latest blogpost in the AStretch 2020 series. Last month, you heard from the inspiring Marie-Therese McDonald about the ‘five reasons people with Axial Spondyloarthritis (AS) might not do physiotherapy exercises and what might help’. In this blogpost, I will introduce some opportunities digital health practice may present in supporting adherence to treatment including exercise.What problem(s) are we trying to solve with Digital Health in Rheumatology? I work in a busy rheumatology service, like many of you. Patients with inflammatory arthritis, including Axial Spondyloarthritis (AS), make up the largest group of service-users. The reality can mean long waits to be seen with clinic flow reliant upon well patients. Given the primary purpose of a rheumatology out-patient appointment is ongoing specialist input for a long-term condition: How much of this input needs to be delivered in an out-patient setting? How much of the important education and exercise guidance frequently delivered by rheumatology physiotherapists is currently delivered remotely (or could be) through the use of digital technology? There have been articles written about singing and its positive effect on our physical and mental health. The release of endorphins certainly plays its part, the work out another. So too does being part of a group of people with the same passion. If you are thinking about singing in a choir or a chorus, it has to be worth a try. The physical, emotional and psychological benefits can be dazzling. What problem(s) are we trying to solve with Digital Health in Rheumatology? I work in a busy rheumatology service, like many of you. Patients with inflammatory arthritis, including Axial Spondyloarthritis (AS), make up the largest group of service-users. The reality can mean long waits to be seen with clinic flow reliant upon well patients. Given the primary purpose of a rheumatology out-patient appointment is ongoing specialist input for a long-term condition: How much of this input needs to be delivered in an out-patient setting? How much of the important education and exercise guidance frequently delivered by rheumatology physiotherapists is currently delivered remotely (or could be) through the use of digital technology? There have been articles written about singing and its positive effect on our physical and mental health. The release of endorphins certainly plays its part, the work out another. So too does being part of a group of people with the same passion. If you are thinking about singing in a choir or a chorus, it has to be worth a try. The physical, emotional and psychological benefits can be dazzling.
Digital health offers a new dimension for rheumatology patient care. Overcoming the constraints of distance, location and time by deploying technology offers considerable benefit to both service provider and user in supporting care from within the home or at work. Despite this tantalising opportunity, patients and clinicians generally make poor use of digital technology to manage healthcare. Understanding this is critical in overcoming the challenge for better use. What is Digital? To understand the impact digital health could have in rheumatology care, we must first understand what ‘digital’ means? Digital is “applying the culture, processes, business models and technologies of the internet era to respond to people’s raised expectations” (NHS Digital). Mobile devices are used on a daily basis to manage many aspects of our lives including travel, finance and social. Yet when it comes to our health we are playing catch-up. The challenge of transforming care through digital is not technical, it is organisational. It is about changing the way we work. Our working culture. I will focus on four key areas where rheumatology could harness the benefits of digital health to support how we might deliver care. Telemedicine Whilst the overarching aim of the NHS Long Term Plan and The Topol Review are to redesign how out-patient care is delivered in the digital era, rheumatology appointment planning remains relatively arbitrary. It is a challenge for rheumatology services to identify which patients would benefit most from more flexible appointment scheduling e.g telephone, video or face-to-face follow-up. Telemedicine can offer a flexible and responsive service model to manage a fluctuating and unpredictable disease such as AS. However, it is important to acknowledge concerns that technology does not come at the cost of humanity but rather “remote access will change clinician’s relationships with patients for the better” (Matt Hancock at the King’s Fund Digital Care Conference, 2019). From my own experience of embedding electronic PROMs into routine rheumatology care, the capture of PROMs prior to clinic attendance has brought about three frequently encountered benefits: 1. As a clinician I am able to prepare better for a consultation and focus on the main issues e.g fatigue. 2. Patients report they take time to complete the PROM and think about what may have caused a change of symptoms – without feeling rushed to complete it in clinic 3. Patients see a clear link between the information they provide impacting on the decisions about their care. There are a number of resources emerging to support clinicians to develop the skills and confidence to lead telemedicine clinics. Why not watch this video for some practical ideas http://bit.ly/nonF2Fclinics
Remote Monitoring The use of digital technologies for remote monitoring in rheumatology has the potential to empower patients to monitor their health outside of the traditional face-to-face setting whilst providing clinicians with meaningful data to support shared clinical decision-making. The proposition of remote monitoring is twofold: To offer more flexible care to the right person at the right time e.g when in flare. Secondly, to support more flexible appointment scheduling, including appointment deferment for whom an annual review is sufficient. However, there is a current practice gap between the use of paper-based PROMs collected in clinic and the timely remote capture of data when it really matters. I am currently involved in a project setting up a new remote monitoring service in rheumatology. In builds on the everyday practice of text messaging. Patients are sent a PROM each month via text message. Patients can also text into the service if they feel they need support between appointments. There have been high levels of engagement with a remote relationship between patient-provider being developed through data-sharing. A future focus of this project will be to understand the impact on clinical outcomes of providing care remotely and the behaviour of both patients and providers in utilisation of rheumatology appointments. What have patients told us about this new service? “Getting the text from you gave me the confidence that the right thing to do was to contact the service, to know I wasn’t wasting anyone’s time.” “I have many mini-flares and know the pattern of these and usually wait for these to settle. I generally know when treatment needs escalating.” To read more about this project visit: http://bit.ly/TopolFellowMM. For further examples of remote monitoring models, why not watch this short film about the REMORA study: http://bit.ly/RAREMORA Health behaviour change & self-management
 Self-management describes an individual’s ability to manage the symptoms and treatment of a chronic condition, in addition to the psychological, social and lifestyle consequences. With AS this can mean having to manage fatigue, pain, stiffness, work impairment and mental health problems on a daily basis. For self-management to be successful, engagement in active health behaviour change may be required. Examples of health behaviour include smoking cessation, increasing physical activity levels and engagement with regular therapeutic exercises. The use of the NHS website www.nhs.uk to ‘prescribe’ high quality health behaviour advice and signposting to the National Axial Spondyloarthritis Society www.nass.co.uk is a really great place to begin to support self-management. I have been involved in the development of the Axial Spondyloarthritis Know-How (ASK) self-management programme as an example of how digital has been harnessed to engage and support self-management of AS. The ASK digital toolkit comprises a short film viewable before attendance to a group education and exercise workshop. Patients view the film in order to manage their expectations of the group intervention and rate the film highly in supporting attendance. The toolkit also includes an interactive PDF self-management handbook which patients can use to record, reflect and refer to a range of resources to support problem-solving, goal-setting and health behaviour change. Patients have continued to use the self-management handbook, choosing either mobile, tablet or computer to continue engagement with the ASK resources following attendance. ASK was awarded the British Medical Association Patient Resource of the Year 2019 on the basis: " Although it (ASK digital toolkit) is designed to be used in conjunction with attendance at a physio group session it deserves a much wider rollout potentially to all patients in the UK with the condition. The digital format should make this easily achievable. It could also provide lifelong support for the patient to record, reflect upon, and monitor their illness and empower their self-sufficiency. This is an ambitious and exciting toolkit." Click here to watch a short film about ASK: http://bit.ly/ASKFilm. Wearables & Apps Rheumatology has seen advances in the development of a number of mobile applications (apps) to support self-care. The apps frequently have the ability to track and monitor PROMs, mood, physical exercise, sleep and other lifestyle factors. An example is the MySpA app where patients can upload an exercise video or photo into a ‘library’ adding to prescribed exercise within the app. Wearable devices also offer an opportunity for patients to track and monitor physical activity levels in accordance with national recommendations. There is also an opportunity for activity tracker data from wearable devices to have meaning in a clinical context, for example, in a study by Gossec et al 2019 explored remote monitoring of physical activity as a predictor for flare in AS. Read more here: http://bit.ly/ASWearables. The exploration of activity levels and disease activity is clearly an exciting area for rheumatology physiotherapists who frequently prescribe exercise as a disease-modifier. Digital Health opportunities are plentiful in rheumatology. Rheumatology services can achieve the flexibility many patients with long-term conditions want if they begin to think digital-first for the prevention, monitoring and self-management of many rheumatological conditions in the digital NHS of the future. Thank you for reading 
Mel
|