The therapy cohort commonly uses Swiss or round shaped Gym balls to improve one’s balance and core strength. Gym ball work by forcing the body to balance against the ball's instability, leading to greater muscle activation. In my experience of using such supportive devices, patients relax and self-exercise easier. Unlike the spherical-shaped Swiss ball, PeaNut shaped (PNS) gym balls offer a slightly more supportive rehabilitation environment. PNS Gym balls are ideal for various therapeutic uses in both children and adults (including the antenatal cohort). The shape offers greater stability and control by limiting movements experienced to just the one axis (forward and backward), Ideal for anyone who requires lateral stability. They are adaptable and offer extra support during exercises improving one’s flexibility, strength, balance, coordination, posture, and mobility. They are extensively used for therapeutic activities including, yoga, Pilates, Taichi, pregnancy and dance. They can be used both in and outdoors. Some PNS balls are manufactured with tactile nodules for massaging purposes, users have reported they are effective in relaxing upper trapezius and scalenus (the most common to get stressed muscle groups).
Research Background Lumbar stabilization exercises sat on a ball iare reported to be effective for alleviating LBP and could produce a higher rate of increase of bone mineral density compared with lumbar stabilization exercises done on the floor (Yoon et al 2013). Recently Liam et al in 2023, identified joint mobilization, breathing works alongside gym ball assisted exercises improved respiratory pattern abnormalities and joint position sense in persons with chronic LBP. Progressive muscle strengthening exercising with assistance of a Swiss ball was demonstrated to be effective in reducing disease activity, improving overall muscle strength, walking performance and great customer satisfaction in patients with Axial SpA. Future studies of longer duration should be attempted to finalise the effectiveness of the Swiss gym balls.
There is limited research surrounding the use of the PNS ball in musculoskeletal physiotherapy. Most of the research done on the PNS balls were aimed in its use during labour. In 2016, clinicians have proved PNS balls compared to Swiss balls were easy tools to measure, assess and improvise trunk extensor’s endurance amongst healthy subjects. Though PNS gym balls efficiency needs to be further evaluated amongst people with inflammatory conditions, one cannot avoid that they are easy to use supportive tools that clinicians can incorporate in testing and in clinical progression training.
PNS Gym ball at our NLAG NHS Trust
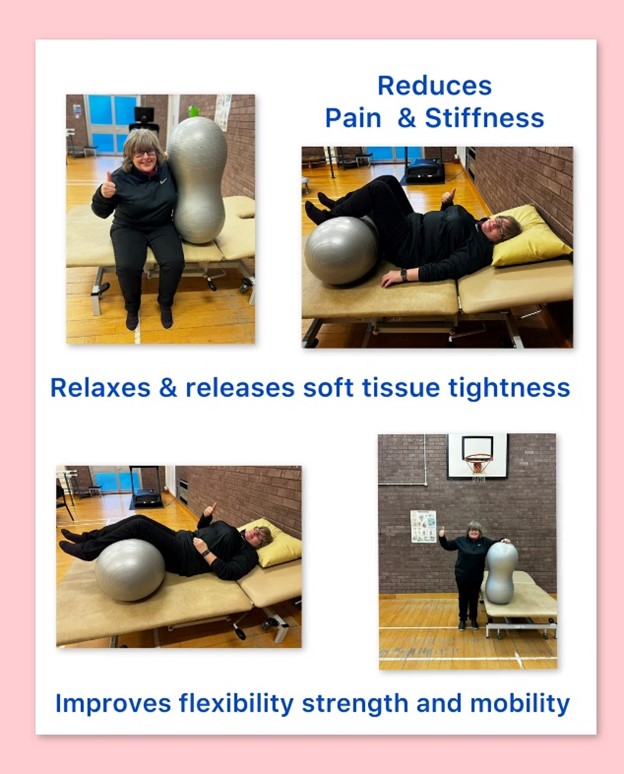
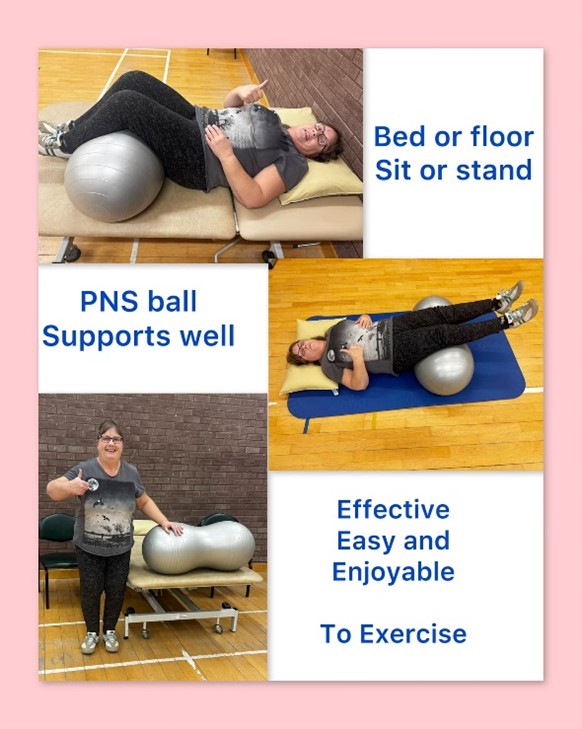
People diagnosed with Rheumatology conditions including axial SpA can struggle to lie/ stretch down regularly for both resting and exercising lower limbs and trunk. Regular gym balls supported resting positions and allowed easier movements of the lower limb/trunk only if the patients can flex their hip/. knee joints beyond > 60 degrees. Introducing PNS gym balls made a significant difference. Only 45 degrees of hip flexion was required to place their legs (compared to the 60-90 degrees required with the Swiss gym balls) and the ridge between the double ball shaped balls worked out as a great supportive platform for both the knee joints and lower limbs.
For the last decade, I have observed the PNS gym balls eased and enabled my patients with rheumatological conditions (who struggle with symptoms with pain /stiffness and fatigue) to exercise easier. The gentle rocking and bouncing of the ball can help regulate ones’ nervous system and promote relaxation and focus. Additionally due to being offloaded, positioned in a flattened lumbar lordosis (posterior pelvic tilted) position, patients with LBP and lower limb related pains can relax and work gradually to regaining the full range of pelvic tilts. Patients instantly report how ‘easier’ it feels using the PNS ball and how the weight of the lower limb been lifted off, reducing the soft tissue strain, thereby reducing further LBP, and associated hip joint pains.
We have been using this PNS ball with axial SpA patients in the earlier pain/stiff days to encourage with the aim of trying to recruit lower trunk and hip/knee joint flexibility, strength, and core stability. The comfortable and easier exercising enabled patients to feel pain less, encouraging them to buy their own gym balls and start self-managing and working through progressions / regressions as per their pain levels. Over the time, patients wean off the ball support and work on their Axial SpA specific home exercise programme. They are happy to self-manage their flare up days using the PNS ball as required.
Patients with axial SpA in NASS group have always reported positive feedback to me:
· Forgot my LBP, I would not mind lying down now.
· Wow, I love this position, it is easier to rest.
· That feels so nice, the weight of my legs has been taken off.’
· I can move my Hip/Knee joints can move without any discomfort.
· Brilliant calm therapy, able to breathe deep with less pain.
Two of our Grimsby Town NASS group members, Sue C, Sue B have used the PNS balls for few years and offered to convey their positive experience with picture illustrations.
Conclusion:
· Improved Outcome measures – active range of movement, muscle power, balance and coordination and pain relief, VAS pain/stiffness/fatigue scores, EQ-5D-5L,
· Improved Patient engagement, compliance, and satisfaction with therapy
· Thousands of patients with rheumatological conditions and several local Grimsby Town NASS group members have bought their own PNS gym ball – because it supports to exercise easier during painful/stiff days. So, they engaged, self-managed symptoms better, progressed easier with further strengthening programme under therapists’ guidance.
· Future trials should evaluate PNS balls efficiency in patient diagnosed with axial SpA.

Susi
References
Yoon, J.S., Lee, J.H. and Kim, J.S., 2013. The effect of Swiss ball stabilization exercise on pain and bone mineral density of patients with chronic low back pain. Journal of physical therapy science, 25(8), pp.953-956.
Chalana Duarte de Sena Fraga et al (2024) Use of a peanut ball, positioning and pelvic mobility in parturient women shortens labour and improves maternal satisfaction with childbirth: a randomised trial. Journal of Physiotherapy 2024 Apr;70(2):134-141.
Nuno Pina Gonçalves et al (2019) The effects of physical exercise on axial Spondyloarthritis - a systematic review ARP Rheumatol 2023 Aug 27.
Patel, G. and Deshpande, V., 2019. Effectiveness of Swiss ball Exercises and Mini Stability ball Exercises on core Strength, Endurance and Dynamic balance in Mechanical Low back Pain. SCOPUS IJPHRD CITATION SCORE, 10(5), p.70.
Lim, C.G., 2020. Comparison of the effects of joint mobilization, gym ball exercises, and breathing exercises on breathing pattern disorders and joint position sense in persons with chronic low back pain. Physical Therapy Rehabilitation Science, 9(1), pp.25-35.
Beate Carriere(1999).The ‘Swiss Ball': An effective tool in physiotherapy for patients, families and physiotherapists, Physiotherapy Volume 85, Issue 10, October 1999, Pages 552- 561
Marcelo Cardoso de Souza et al (2017), Swiss ball exercises improve muscle strength and walking performance in ankylosing spondylitis: a randomized controlled trial Revista Brasileira de Reumatologia (English Edition)Volume 57, Issue 1, January–February 2017, Pages 45-55
Tarek M. El-Gohary et al (2016): Using the Swiss ball versus peanut ball to assess the back extensors endurance among healthy collegiate physical therapy students at Taibah University International Journal of Therapies & Rehabilitation Research, January 2016
Alice Goodman (2013): Exercise Improves Outcomes in Ankylosing Spondylitis Medscape Thursday, November 21, 2024